A Deeper Look at Narcolepsy Through the Eyes of the Afflicted
When Keith Rubenstein’s problems with sleep first reared their head, almost four decades ago when he was just a teenager, they were dismissed as typical youthful laziness. Rubenstein’s inability to stay awake in classes was attributed to little more than boredom. He began to find any excuse to skip classes simply to avoid falling asleep at his desk, an amble he took so often, his classmates voted him “Biggest Hall Roamer” his senior year.
It wasn’t until Rubenstein turned 43, however, that he really began struggling with sleep: the inability to get very much sleep at night, coupled with a feeling of persistent sleepiness. Says Rubenstein, “It’s not exhaustion, it’s not fatigue…it’s sleepiness.” He began to doze off at work, often in short intervals, unable to recall what he had just been doing. Yet at night, the sleepiness would seem to evaporate, leaving Rubenstein with restless sleep that only further fueled the inability to keep his eyes open during the day.
It’s now been six years since Rubenstein was diagnosed with narcolepsy, and like many other narcoleptics, he’s found a cocktail of remedies, both medicinal and changes to his lifestyle, that help alleviate his symptoms. Yet there’s still no cure for narcolepsy, which is why Rubenstein is so passionate about helping others manage a widely misunderstood disorder.
Diagnosis
Narcolepsy has an incidence rate of 1 in 2,000 people, affecting roughly 200,000 Americans and 3 million people worldwide. Major symptoms include an uncontrollable urge to sleep at inappropriate times, a weakening of muscles that can lead to a person sagging over, poor nighttime sleep quality, sleep paralysis, and vivid hallucinatory dreams. Not all narcoleptics exhibit all five symptoms, and the intensity of symptoms can ebb and flow over time, making narcolepsy even more challenging to diagnose.
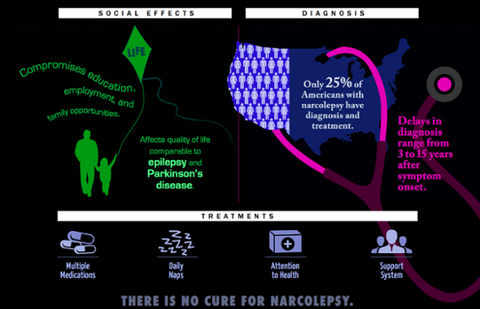
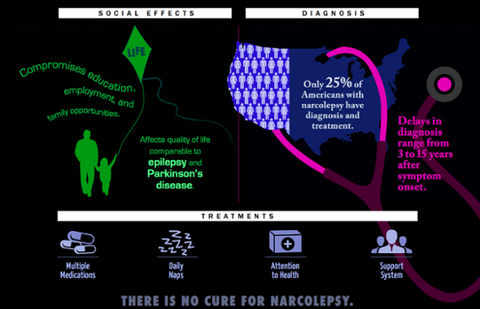
Despite the prevalence of narcolepsy, the sleep disorder remains largely misunderstood, even by physicians. According to a 2012 study done on narcolepsy diagnosis rates, while 62% of sleep specialists felt comfortable discussing narcolepsy, only 42% felt comfortable enough diagnosing patients as narcoleptic. But sleep specialist referrals generally only come after a patient has talked to their primary care doctor, and as the study found, only 24% of primary care physicians felt comfortable discussing narcolepsy with a patient. When it came to actual willingness to diagnose? Only 9% of primary care physicians felt comfortable doing so. This opacity around narcolepsy, even within the medical community, has become so prevalent that researchers estimate that only 25% of narcoleptics are ever formally diagnosed.
Rubenstein was one of the luckier ones: two prominent Chicago hospitals both diagnosed him as a narcoleptic, along with obstructive sleep apnea, a sleep disorder affecting the breathing of over 3 million Americans, and a third form of REM sleep disorder.
“I was diagnosed with narcolepsy by two prominent Chicago hospitals and I still didn’t believe it,” says Rubenstein. “I spent a week at the Mayo Clinic, really going through [all] the tests and they [told me] to stop checking. I have it.”
Depending on how you look at it, Rubenstein is one of the lucky ones. While his teenage sleep issues now appear as clear indicators of narcolepsy, which often starts during the teen years, he was able to manage his symptoms. And when they began six years ago for him, doctors were able to diagnose the issue fairly quickly. For most narcoleptics, the condition can go through a series of misdiagnoses, including fatigue, depression, and obstructive sleep apnea (the latter of which Rubenstein does have). The average period of time from initial symptom to accurate diagnosis for narcoleptics is closer to six years.
Narcoleptics are often found to have a lack of hypocretins, a brain chemical that essentially interferes with the function of the brain’s “on-off” switch. While understanding the loss of hypocretins is a major breakthrough, the specific mix of genetic and environmental causes remain unclear. Yet the scientific breakthroughs are only a mild comfort to narcoleptics like Rubenstein at this moment; the disorder is a chronic condition. It can only be managed, never cured.

Day-to-Day
Diagnosing narcolepsy is only a small part of the battle. Treatment can often be only mildly effective, which makes managing day to day life in challenging. Rubenstein’s narcolepsy most often comes in the form of what he calls sleep attacks. “It’s a sudden strong onset of the feeling that your brain is almost forcing you to lie down and sleep,” explains Rubenstein. “My voice gets raspy, my eyes water, I [become] weak.” His sleep attacks would hit throughout the day: during meetings, especially if lights were turned down, while spending time with his family, and even while driving.
Rubenstein, like many other narcoleptics, also experiences micro-sleeps, where he briefly loses consciousness for about 10 seconds, often with little memory of the conversation he had just been in. But his sleep attacks also sometimes manifest as cataplexy, a symptom of narcolepsy more in line with the exaggerated Hollywood portrayals of someone dramatically falling asleep mid-sentence. While narcoleptics who also suffer from cataplexy don’t quite fall face first into their soup, it does cause a loss of muscle control, which can be as simple as falling asleep with their head on their shoulder, or slumped down in a chair.
While Rubenstein’s days were characterized by a pervasive sleepiness, his nights were often restless. “Being sleepy for a narcoleptic, we’re told by experts, is akin to a person without a sleep disorder staying awake for 72 hours. That’s how sleepy many of us feel each day, no matter if we sleep eight hours or two.” Yet Rubenstein often slept erratically, which only exacerbated his sleep attacks during the day.
His lifestyle began to change also: keeping a schedule became impossible, as waking up is no easy task. “Mornings are extremely challenging. I can wake up, do my prayer and meditation routine, shower, and instantly need to fall back asleep. That’s the worst of worst feelings for me, [and] it happens whether I’m on [sleep disorder] medications of not.”
As a CEO of his own medical ultrasound company, Rubenstein found himself walking around often, in a fast-paced environment he likens to traders on stock exchange floors. He credits his staff for being patient as he acclimated to the realities of his sleep disorder, especially as the day-to-day realities for someone with narcolepsy can change on a dime. When I ask Rubenstein what a perfect day would look like without sleep issues, he sums it simply. “I don’t have perfect days relative to sleep issues.”
Shop All Standing Desks
Management
Many narcoleptics use a variety of prescription stimulants, including dexamphetamine and modafinil, to help manage symptoms and keep themselves awake. Yet the medications can often be only partially effective, and can have adverse side effects after prolonged use. Modafinil in particular has been shown to reduce creativity and flexibility of thinking in regular users.
Rubenstein has tried a number of therapies to ameliorate his sleep issues, including gluten free diets, regular acupuncture, holistic medication, and support groups. Over the years he found a few solutions that yielded semi-consistent results: taking his prescribed meds regularly, and sleeping and waking at the same time. He’s cut out alcohol, and added in exercise and healthy eating to his nutrition plan.
Two of Rubenstein’s biggest sleep attack triggers are stress, and repetitive actions. Because of this, he tries to minimize his stress levels, and the amount of busywork he engages in. He also says that sticking to a routine is the best thing a person with narcolepsy can do – a goal he tries to stick to as often as possible, though late night bursts of insomnia can throw a rock into those plans. His daily routine involves waking up, spending some quiet time looking at a Philips Brite Lite, a tool suggested to him during his time at the Mayo Clinic to help regulate his circadian rhythm, which keeps his sleep-wake cycle functioning regularly. He makes his kids breakfast before getting ready and heading off to work, where he has to keep himself constantly moving – even while eating lunch – to stave off sleep.
While his scheduled routine and mix of alternative and medicinal therapies helped, Rubenstein always felt that sleepiness was present in the background, and he continued to look for therapies that might abate some of his exhaustion. Narcolepsy sufferers on forums had been mentioning that standing up helped them stay more alert while working, though many were using homemade rigs. Rubenstein instead purchased an automated standing desk from StandDesk, which he says has made a significant impact.
“I knew there had to be a better way to keep me up all day. Once the desk was delivered, I fell in love with it. It makes it nearly impossible to fall asleep while working,” says Rubenstein, who has also added a treadmill underneath his standing desk. “The standing desk was the best solution I’ve tried, and is the single best thing I have aside from medicine that helps me. It keeps me awake better [than other therapies]. I may get a sleep attack and have to sit or lay down, but it’s far less frequent with a standing desk. It’s also a piece of art. It gets compliments from clients worldwide. I bought one for my COO, who loves it as well. He says he feels healthier using it.”
Perception
Though Rubenstein has found solutions that help keep him alert, he says the public perception of narcoleptics can always be difficult. Movies like Moulin Rouge and Deuce Bigalow: Male Gigolo, and TV shows including The Simpsons, Modern Family, and Arrested Development have all featured narcoleptic characters – often in humorous guest roles that involve a person falling dramatically asleep, before crashing to the ground. Yet narcolepsy, even in those who experience cataplexy, can be hidden. Says Rubenstein, “Often we’re in a state of being awake and asleep at the same time, and [people] don’t even know it.”
He says that managing a silent disease can be challenging. “Most of us look ‘normal,’ dress normally, and don’t have tubes in us. We aren’t famished looking.” People can mistake narcolepsy for laziness, and often times, even well-intentioned suggestions can minimize the depths of his sleep disorder. “So often family members or friends will make suggestions like, ‘Take a nap!’ or ‘Drink more coffee.’ They mean well, but it’s so much deeper than that.”
Nowadays, Rubenstein manages his narcolepsy with medication, a prescriptive routine he follows as best he can, and his standing desk. Though all three have helped significantly, there’s one more tool that Rubenstein credits as essential to helping manage his narcolepsy: acceptance.
“When I accepted the sleep issues a few years ago instead of questioning ‘Why me?’ or ‘Of all things to get, narcolepsy,’ [things got better].” He now uses prayer, gratitude, and an attempt to defocus on his disease, and says the attitude shift has changed immensely. Though we’re chatting at 11 PM, and Rubenstein has assured me he’ll be up for hours, for once, it’s a good sign that I don’t have an interviewee’s full attention.
“Truly this attitude change has helped,” says Rubenstein, “but I’m really dozing off as I talk to you.”
Want to build your own standing desk? Check out this link to find the Standing Desk that works for you:
Shop All Standing Desks